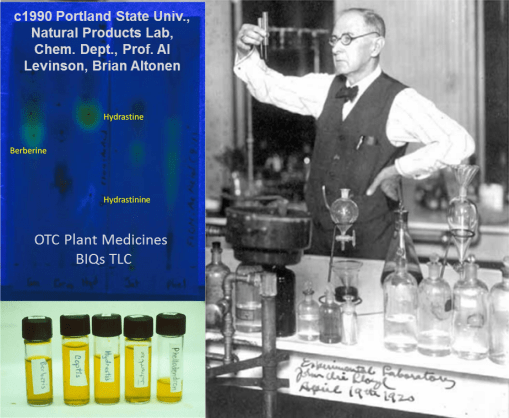
Over the last 6 or 7 years I have been “showing off” this algorithm I designed nearly a decade ago, longer in terms of copyright and intellectual property rights claims.
This way of modeling disease patterns is a direct product of my first studies of spatial data, which ironically focused on remote sensing and the value of raster imagery before I was able to see the value of a standard point-line-arc or point-line-polygon geographic information system (i.e. the ESRI and MapInfo GIS products from the mid 90s).
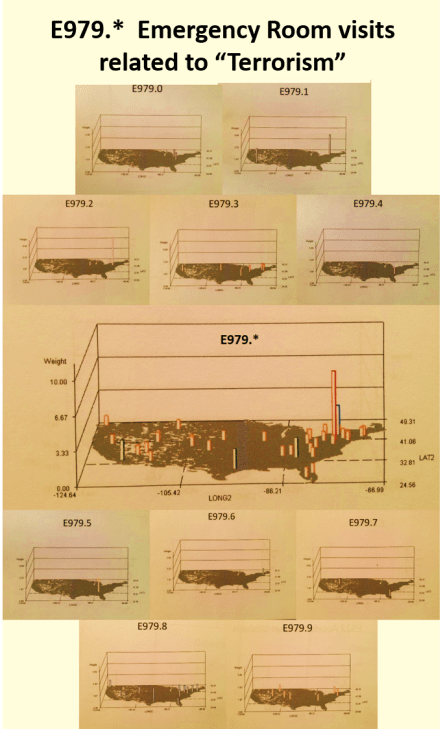
When I developed my first algorithms, they were for differentiating land use patterns, in particular regarding vegetation types and the patterns changing “browns” and “greens” they produced in the various early Landsat and AVHRR imagery then available for research. I came up with/developed and tested some unique algorithms for overlaying trend surface models to identify important edges to overland diffusion processes, such as for a migrating animal bearing disease, or a pathogen capable of spreading as wind-blown materials. I even used these to study the nature of very large repeated forest fires developed due to a combination of climatic, meteorologic, topographic and phytochemical (resin index) features. These algorithms were used to exaggerate 3D differences, converting them from linear to logarithmic in order to depict the most important “hot spots.”
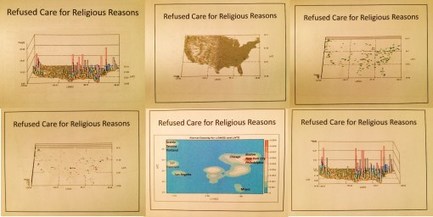
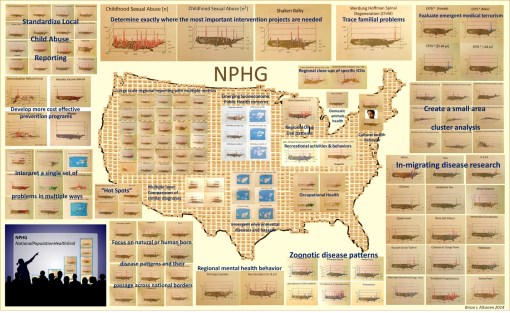
Later I found a use for these algorithms in evaluating population density, public health related features. The same algorithms that defined edges for conifer rich regions in the mountains could be used to define religious, cultural, age pattern density, environmental disease, elevation, traffic flow, and sociocultural disease type edges. The edge of outbreak and outbreak susceptible areas can be defined quite easily using mixed 2D and 3D modeling.
You can also overlay certain features on some of these diagrams that can be developed in the right SAS programming (not at all requiring SAS GIS). These features include risk area patterns, critical p lines demonstrating the edge of a break out area, points depicting where the event peak is relative to local police and fire stations, a hospital, an emergency care facility, a specialty clinic in charge with specific public health concerns.
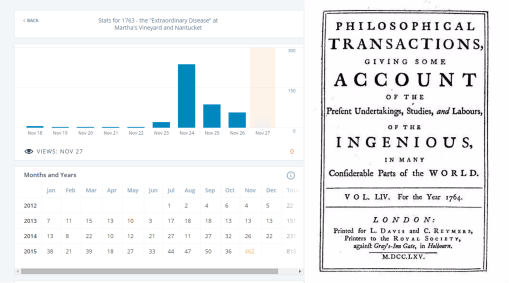
The amazing thing is that today, with the current technology, without ArcGIS, QGIS, Cognos, Tableau, these maps can be produce, in record amounts per day. All of the 45-60 Meaningful use (MU) metrics can be evaluated several ways (by facility, by race, by ethnicity, by clinic, by provider, by provider type, as percent performance) in a single run of the program, using the right macros.
In a regular Data Warehouse, it takes a day or more to develop the macro from scratch. But then, once it is finished, it is written such that it can be applied to other metrics. The process for using a macro-based process for running your daily ED evaluation or weekly MU review, cost analysis, enables up to 2 or 3 hundred tests to be run in less than two hours. In terms of 3D modeling, producing multiple images of the same result, depicting the same finding but at different rotational angles, it takes a few minutes more to produce several maps, a half hour more to produce hundreds of them.
What takes the most time right now at this end for mapping diseases and health / visit behavior is the time to pull the data (it sometimes take just as long, a half hour to a few hours, times 5 or 10 on occasion).

On a good day, I have found that one can spend 3 or 4 hours writing up the logic, the sql and SAS needed to pull the data and reassess it, resort it, count it out, in such a way as to produce your numbers. Add another half hour to merge this with your overall population data for comparisons (i.e. for incidence/prevalence measures), and if necessary link as well any additional spatial data required by your facility for the areas to be assessed (i.e. pull in zip code data for: facility, special location, and even patient residence for proximity to care measures).
A great program in managed care, that implements GIS and spatial analysis, is productive in 3 months at the demographic, basic numbers level. It should be producing spatial data (maps or the likes thereof) in 4 to 6 months. Depending upon the software used for GIS (which is not required so far), another month or two is needed to develop the actual GIS tool process for a standard coarsely mapped zipcode or county (even census block or clock group) based system.
- A GIS based managed care system should be able to engage in meaningful use related activities such as:
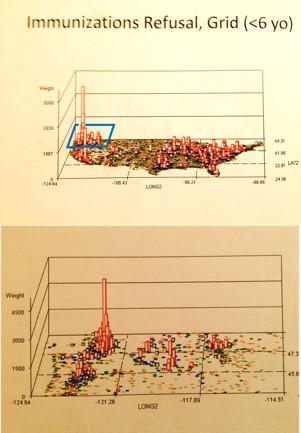
- location analysis of 0-2 yo immunization completion findings,
- develop of a clustering algorithm for mapping asthma and COPD patients,
- engaging in a study of relationships to completion of well visit requirements relative to facility types and service hours
- mapping suicide attempt rates (V and Ecodes), as an age-gender-race metric
- developing comparative studies of cancer risk testing rates at the socioeconomic level,
- evaluating STD spatial distribution relative to age group and ethnicity
- documenting diabetes prevalence rates for specific zip code defined areas
- documenting the distribution of spouse abuse events in EMR derived by Ecodes information
- relating SES and median income to costly chronic disease medication timely refill statistics
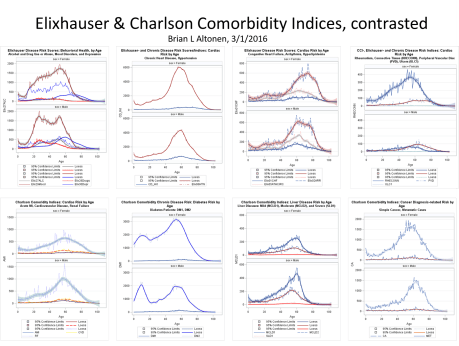
- producing areal maps of immunization refusal family clusters based upon Vcodes
- mapping zip code or retirement facility specific overall health risk in 3D, based upon Charlson comorbidity (CCI), Elixhauser comorbidity and federal Chronic Disease Management algorithms.
There are three major stages or series of processes required to develop a spatial GIS for managed care. I have identified these as EMR, Spatial, and then GIS stages.
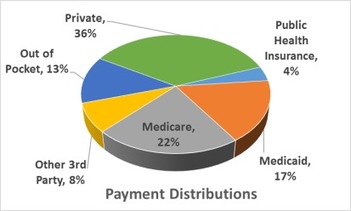
The EMR Stage is the development of data into a usable form for spatial analyses. Nearly all managed care facilities have the goal of reaching this stage in their development. A few programs even implement some form of Cognos, Tableau, ESRI tool, QGIS, or the like, for information mapping. Information mapping is different from Spatial Analytics mapping.
There are a number of places that engage in pseudo-spatial mapping. They analyze data by simple areal and point features (EpiINFO / EpiMAP style of work), don’t actually engage in spatial analysis, but spatially present their findings. Some even use these products to design special needs or intervention programs. If a pre-post evaluation is performed, the spatial process is well on its way to being implemented as a standard part for a Managed Care program.
One level above this pseudo-spatial analysis is using spatial techniques with a spatial purpose. Like developing a spatial data program that utilizes zip codes to define areal risks based upon age-health features, and then using the spatial process to define cluster areas or predict where the next clusters of cases will emerge, such as new diabetes patients over 65 or more cases of toxic lead paint exposure in low income urban settings.
Proactive use of spatial methods in an essential part of the true spatial analysis routine. Reactive or retroactive spatial evaluation are simply that–a review of the past, but without a particularly well defined reason other than to better understand an event. In the west nile example I engaged in more than 10 years ago and posted, I used GIS (but spatial processes) to evaluate west nile clusters of positive testing hosts and vectors, then set traps to prove that a local vector existed at the nidus of spatial centroid of that area, and then used that area to demonstrate that the mosquito carrying this disease could survive the following winter; which it did, enabling me to come up with the first early Spring positive testing sample. (I have a page or two posted on this.)
In sum, the spatial process of spatial analytics development within a managed care system involves understanding and employing your spatial formulas, even though your company may not be regularly using a GIS to meet its requirements.
Spatial techniques may also, incidentally, be used to evaluate SES, demographics, marketing, cost performance, fund raising program success, public interaction of the healthcare program or facility with the local populations. Spatial evaluations of this sort are often requested, but often by engaging outside resources to provide the mapping and analytics required, due to the cost of the staff and hardware associated with this form of productivity.
Spatial analysis at the institution. health care level is reached when data is functional and used by a facility, from its EMR warehouse. These uses includes areal analyses of some sort, engaged in regular, and as part of occasional or once only programs such as for a grant funded research. Forward thinking is also required for a spatial analysis program to truly be engaged. This means that production at the next stages need to be ongoing, with regular presentations provided at times to inform the right people. Presentations at local meetings and conferences are also essential to making the program stable, ongoing, able to discover more areas of interest in need of research, more groups of people and npos that can benefit from continuing the program, and more followers at the production and performance level, including other workers with similar skillsets and their own unique spatial analysis abilities.
The third stage, or GIS stage, of this setting, occurs when an actual GIS is incorporated into this process, not just for demonstrating results in a report, but for use in analyzing specific questions, completing analyses that cannot be easily performed in the spatial tools that do not map (prediction programs that calculate probability, but don’t map; SAS generated tables and charts, but not maps). Two forms of GIS are traditionally recognized as applicable to healthcare–the line-vector and the raster system. Both should be available to the managed care system and be used for spatial databasing, operations development (testing and designing algorithms specific to your program), presentation (at managerial on down to public levels), prediction modeling, and producing final summaries or atlases depicting your program’s spatial results, for the annual report required of most healthcare systems.
At another site I am working on the details of all of the reporting that can and should be done by a managed care combined EMR-GIS/spatial analysis program (a small part of my dissertation work.)
At several locations I posted examples of many the above mentioned products. (I’ll also try to post some examples here).
[Note: I also have a survey posted at SurveyMonkey, querying those engaged in managed care or GIS and health about their experiences in this field.
Participation in this survey is of course appreciated from this end; it abides by IRB requirements; no personal info is divulged; it exists only due to my work as a leader in this specific epidemiology/population health specialty. Please visit it at https://www.surveymonkey.com/r/JW88X3F ]
This slideshow requires JavaScript.